DiYES International School – Britain’s Youth Health Emergency has reached a critical point as more children flood emergency departments across the country. This surge is not the result of isolated accidents or seasonal illnesses but of a deeper systemic failure. In towns like Blackpool and Cumbria, untreated medical conditions, rising obesity rates, and worsening mental health among children are creating daily pressure on hospitals. Parents now often turn to emergency care for issues that should be handled in primary care settings. NHS records confirm that as community health infrastructure weakens, hospitals have become the default for vulnerable families. Meanwhile, overstretched clinicians struggle to respond to both immediate crises and long-term care needs. Without accessible and consistent local services, families lack the guidance and support needed to detect early signs of illness. Despite these challenges, early-stage improvements from nurse visits and community outreach programs suggest that recovery is still possible with strong intervention.
Across the UK, Britain’s Youth Health Emergency reflects broader inequality within the national healthcare system. Children in underserved regions face far greater barriers to care compared to their peers in more affluent areas. Towns such as Blackpool and Cumbria have become case studies in how poverty and underfunded services intensify health challenges. Schools report increasing numbers of students showing signs of chronic fatigue, poor diet, and behavioral distress. With limited access to pediatricians or mental health counselors, many of these children go untreated until symptoms worsen. NHS mobile units and school-based health programs attempt to fill the gap but cannot meet demand. Communities also lack consistent access to nutritious food, safe recreation areas, or preventive care clinics. All of these factors contribute to a system where children from low-income backgrounds are disproportionately represented in emergency wards. This health divide continues to grow unless significant policy and funding changes are introduced.
“Read about: New RSV Shield for Babies: ACIP Endorses Clesrovimab for Infants”
Rising obesity among young people now collides with an escalating mental health crisis, doubling the burden on emergency care. Doctors across England observe a troubling link between poor physical health and emotional distress in children. Obesity contributes to chronic pain, fatigue, and isolation while also exacerbating depression and anxiety. At the same time, young people report intense academic pressure, bullying, and disrupted family life. With mental health services often under-resourced or located far from home, children seek urgent help in hospitals. Some arrive with panic attacks or self-harm injuries that could have been prevented with timely support. School counselors face high caseloads and long referral times. Meanwhile, general practitioners struggle to offer mental health care in short appointments. Without coordinated physical and psychological support, many children return to the emergency room again and again. A more integrated system of care remains the key to long-term recovery.
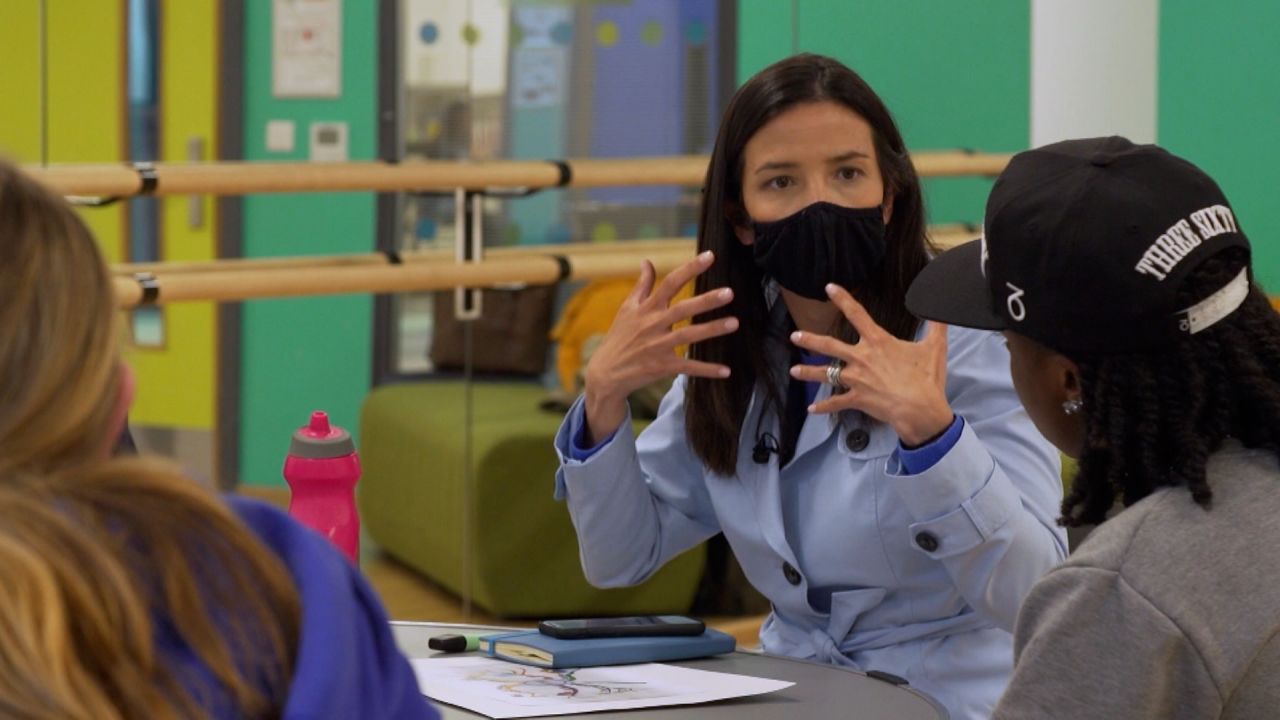
New models of community-based care offer promising signs of change in response to Britain’s Youth Health Emergency. In pilot areas, trained nurses now visit families regularly to monitor health issues and deliver preventative support. These visits help catch early signs of asthma, malnutrition, and developmental delays. Parents also receive guidance on diet, sleep routines, and stress management. In schools, health outreach coordinators educate children about mental well-being and hygiene. These localized services reduce emergency department visits by offering practical care before crisis levels are reached. Collaborations between local councils and NHS trusts make it easier to share data and respond to rising trends. Families benefit from having one point of contact for multiple needs. Though still limited in scale, these programs demonstrate that strengthening local networks directly improves child health outcomes. When families trust and engage with community services, they are less likely to turn to hospital emergency rooms.
“Read more: The Herds Take Over London Streets with a Climate Warning”
The path forward for Britain’s healthcare system must prioritize children by building a stronger foundation in primary care. Stakeholders across health education and local government must work together to scale up successful pilot programs. Investment in school nurses, mobile clinics, and family outreach will address problems earlier and reduce strain on hospitals. Digital platforms that track health histories and coordinate care across institutions are also critical. Parents must receive clear and accessible information about where and when to seek help. Incentives for pediatric specialists to work in underserved regions can close the gap in service access. Most importantly, child health must be seen as a national priority rather than a local issue. When the country supports its youngest generation with strong policies and reliable services, the overall health system becomes more resilient. The time to act is now, before today’s emergency becomes tomorrow’s norm.