DiYES International School – Pulmonary Hypoplasia in Newborns is a condition where the lungs are underdeveloped at birth. This disorder can cause severe breathing problems. It usually appears during fetal development in the womb. The lungs fail to grow to normal size and capacity. As a result, oxygen delivery to the body becomes difficult. Pulmonary hypoplasia often occurs alongside other congenital abnormalities. Early diagnosis can increase the chances of survival. Proper management requires coordinated care between doctors and specialists.
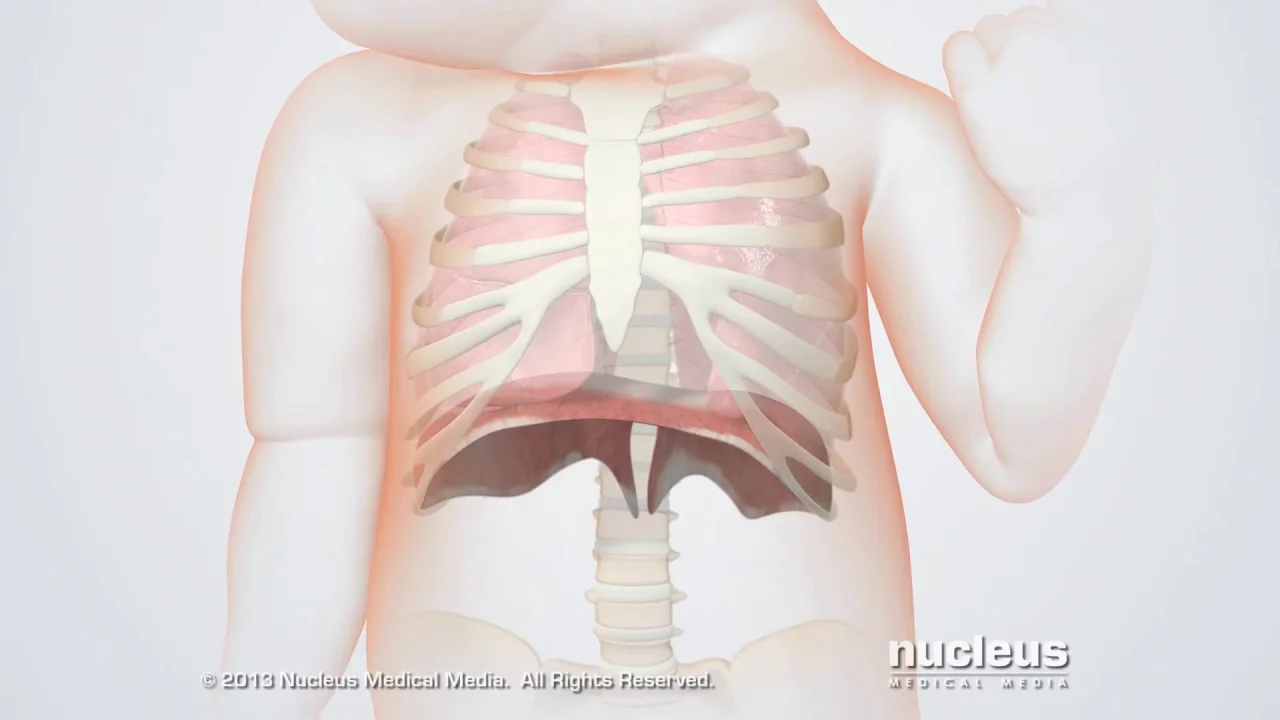
Pulmonary hypoplasia refers to incomplete lung development. It involves a reduced number of lung cells and airways. The lung tissue may also be structurally abnormal. This condition can affect one or both lungs. In most cases, both lungs are affected to some degree. A lack of lung growth limits oxygen intake in newborns. As a result, respiratory distress is frequently observed after birth. Severe forms can lead to life-threatening complications. The condition may result from physical or genetic causes.
“Read about: Down Syndrome: Genetic Condition and the Importance of Early Intervention”
Several prenatal factors contribute to pulmonary hypoplasia. Low amniotic fluid levels (oligohydramnios) are a leading cause. The fluid helps stimulate fetal lung growth. Without enough fluid, lung expansion becomes limited. Congenital diaphragmatic hernia is another known trigger. It allows abdominal organs to enter the chest cavity. This compresses the lungs and restricts development. Skeletal abnormalities such as thanatophoric dysplasia can affect the chest wall shape. These changes reduce the space available for lung growth. Chromosomal or genetic syndromes may also be involved. Infections during pregnancy may impair lung development in rare cases.
Symptoms usually appear immediately after birth. Newborns with pulmonary hypoplasia often show labored breathing. Their chest may appear small and under-inflated. Cyanosis or bluish skin may develop due to low oxygen. Low Apgar scores are often recorded during delivery. Mechanical ventilation is frequently required within minutes. Heart rate and blood pressure may be unstable. Pulmonary hypertension may also accompany the condition. Some infants show little response to oxygen therapy. The severity of symptoms depends on how underdeveloped the lungs are.
Doctors sometimes diagnose pulmonary hypoplasia before birth. Ultrasounds monitor fetal development throughout pregnancy. Medical teams measure lung size while the baby is still in the womb. MRI scans give detailed images of the chest cavity. Doctors track amniotic fluid levels to assess fetal health. After birth, X-rays confirm reduced lung volume. Cardiologists perform echocardiograms to check for heart problems. Medical staff use blood tests to identify infections or genetic concerns. Doctors rarely perform lung biopsies on newborns. Genetic counselors recommend testing for families with risk factors.
“Read more: Evaluating Impact: Frameworks for Monitoring Anti-Trafficking Efforts”
Doctors determine treatment based on how severe the condition is. Mild cases often need supportive oxygen therapy. Moderate cases usually require continuous respiratory support. In severe cases, doctors provide advanced life-saving interventions. Specialists sometimes use extracorporeal membrane oxygenation (ECMO) for critical patients. This machine temporarily replaces lung and heart functions. Physicians prescribe medications to manage pulmonary hypertension. Doctors often use diuretics and surfactants during therapy. Nutritionists ensure proper feeding for optimal infant growth. Surgeons correct any additional structural defects if needed. Pediatric teams provide ongoing care, monitoring, and developmental therapy.
The prognosis depends on the condition’s root cause. Infants with isolated pulmonary hypoplasia often show good recovery. Children with complex defects usually face long-term difficulties. Some children experience noticeable developmental delays over time. Many suffer from recurring respiratory infections during early years. Doctors regularly conduct lung function tests during follow-up visits. Parents often receive training to handle oxygen equipment at home. Medical teams coordinate care to support child development. Specialists provide pulmonary, cardiac, and nutritional evaluations routinely. Counselors offer emotional guidance to help families cope effectively.
Researchers are developing new strategies to improve outcomes. Stem cell therapy is being explored for lung regeneration in cases of Pulmonary Hypoplasia in Newborns. New imaging techniques help detect lung issues earlier during pregnancy. Gene therapy may offer future treatment options for affected infants. Artificial womb technology is under investigation to support fetal lung development. Clinical trials study the effectiveness of new medications on Pulmonary Hypoplasia in Newborns. International registries track long-term patient data and recovery progress. Awareness campaigns help educate parents and healthcare providers. Improved prenatal care reduces the incidence of lung underdevelopment. Non-invasive diagnostics are gaining popularity in neonatal care practices.